Looking for something?
Clinical Trials Begin for Ultra-Rare Treatment of Alexander Disease
It is always exciting to observe phenomenal results in the treatment of a disease in animal studies, and even more so to see them move into clinical trials. ASOs have proven to be efficient at providing deep reductions in disease causing proteins, and a treatment that produced significant results in rats is now entering a clinical trial to treat a devastating neurological disorder called Alexander disease.
Alexander disease is a progressive, ultra-rare neurological disorder that results in severe disability and death. Specific numbers are not available, but it is estimated that approximately one out of every one million babies are born with this condition. Onset of symptoms can be seen in newborns or anytime throughout childhood to young adulthood. Although rare, even older adults may be diagnosed with Alexander disease.
Symptoms vary depending upon the age of onset and may include seizures, physical or cognitive developmental delays, weakness, and an enlarged brain and/or head, muscle stiffness, hydrocephalus (fluid in the brain), feeding problems, and sleep disorders.
Often, children with this disease will display symptoms by the age of 4 (known as Type 1) and earlier onset usually results in more severe disease and survival beyond adolescence is rare. When onset occurs in children over the age of 4 (Type 2), symptoms may be less severe and progress more slowly, although the disease is still devastating. Adult onset usually means that the symptoms will be milder (1).
There is currently no treatment to slow or halt disease progression, but proactive, comprehensive medical care is helpful for those diagnosed with the disease. Various interventions such as physiotherapy, speech therapy, nutrition, and anti-epileptic drugs can help patients maintain the best possible quality of life as the disease progresses.
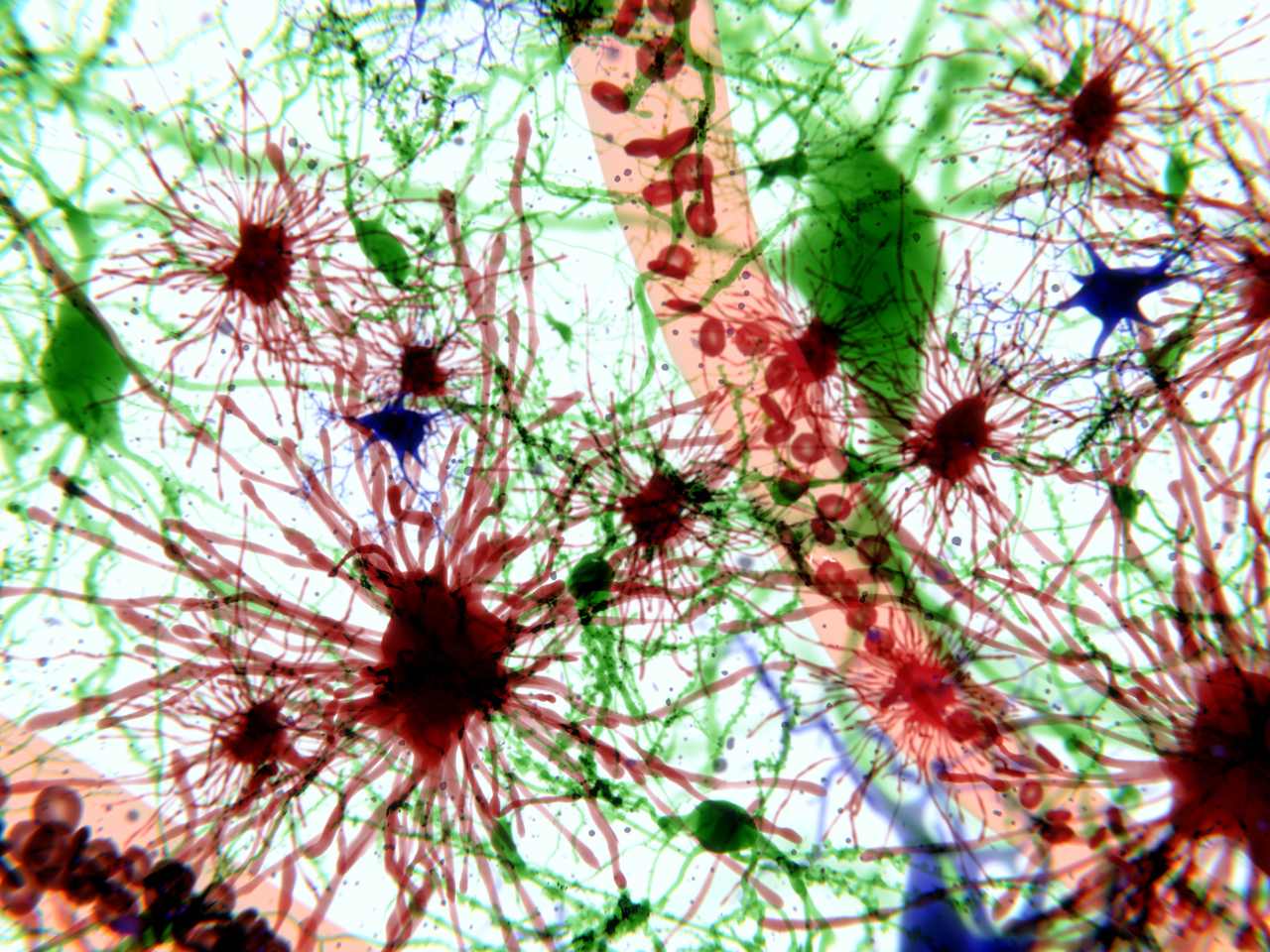
The disease is almost always caused by missense mutations in the GFAP gene on chromosome 17. The mutation results in the overproduction of an abnormal form of GFAP (glial fibrillary acidic protein), which causes Rosenthal fibers (clumps of proteins) to form in the arms of astrocytes (specialized type of glial cells in the central nervous system that outnumber neurons about fivefold) (2). Rosenthal fibers may accumulate in the cerebral cortex, white matter of the brain, brainstem, and spinal cord, causing a toxic effect and leading to the symptoms listed above.
The disease is also characterized by destruction of white matter in the brain and is classified as a leukodystrophy, which is a rare genetic disorder that affects the white matter of the brain. Making everything worse, Alexander disease is a neurodegenerative leukodystrophy, which means that neurons lose their structure and functionality over time, in addition to the loss of white matter (1).
Since most cases of Alexander disease are caused by gain of function mutations and there are over 100 known disease-causing variants (2), antisense oligonucleotides (ASOs) may provide a solution through suppressing and ultimately, normalizing expression of the GFAP gene. ASOs can be designed to bind with specific mRNA (in this case the mRNA that carries instructions of the GFAP gene) and the cell will then destroy the mRNA. If the GFAP gene is not able to be expressed, it prevents the overproduction of the protein so toxic accumulation is avoided. When GFAP is knocked down almost to zero, mice and rats seem to be fine (3) as far as development and reproduction but do appear worse off compared to controls when experiencing some diseases and injuries (4). Deep reductions may keep the disease from progressing and, in the best-case scenario, even reverse progression. For those facing a debilitating disease and early death, the benefits may easily outweigh any potential risks.
Ionis has successfully created an ASO that treats Alexander disease in a rat model which mimics the disease features. The ASO targets and binds to mRNA, blocking production of GFAP. The mRNA target was chosen to serve the broadest possible patient population. GFAP-targeted ASO treatment led to long-lasting suppression of GFAP transcript and protein, and nearly complete knockdown was achieved (4).
Two groups of rats were treated. One when they were 3 weeks old, before the onset of obvious symptoms, and the other group was treated at 8 weeks of age, when they were already severely impaired. In the rats treated at 8 weeks, Rosenthal fibers disappeared within a few weeks of one injection and several markers of the disease returned to levels that are close to normal, even when administered during peak expression of the disease. Some damage in white matter was reversed and symptoms, including motor impairment, improved (4).
If rats were treated at 3 weeks of age, before developing major physical symptoms, they were physically indistinguishable from wild-type littermates as they developed, showing no difference in weight, and white matter did not show deterioration. They also displayed sustained GFAP suppression 24 weeks after treatment (4).
This success has led to a multiple-ascending dose (MAD) clinical trial of ION373. The Phase 2/3 study is underway and is currently recruiting at nine different sites throughout the United States, Canada, and the Netherlands. As many as 58 patients ages 2 – 65 with Alexander disease will receive an intrathecal bolus (ITB) injection of ION373 or placebo once every 12 weeks for 60 weeks (5 doses), then all patients will receive ION373 for 60 weeks during the open label treatment period (another 5 doses for a total of 10 doses or 5 doses of placebo plus 5 doses of the drug).
ION373, which is wholly owned by Ionis, has received orphan drug designation from the EMA (European Medicines Agency) and the U.S. FDA (Food and Drug Administration), in addition to receiving rare pediatric disease designation from the FDA.
While results may not be as drastic in humans as they were in rats, even if it is found that some of the damage is able to be reversed or the progression of the disease can be slowed or halted, this would represent a significant victory in fighting this terribly destructive disease.
In another study that we have posted about previously, researchers used heteroduplex oligonucleotides (HDOs) conjugated to cholesterol or α-tocopherol to allow oligonucleotides to safely cross the blood-brain barrier in mice and cynomolgus monkeys. Although most of the work done in this study targeted Malat1 in the CNS, the team also confirmed that the HDO platform produced a modest but significant gene knockdown of GFAP in the brain and spinal cord. However, the study was too short to evaluate GFAP protein reduction. This may eventually provide another method of treating Alexander disease and other neurodegenerative diseases (5).
It is incredible to see years of research and development now paying off with oligonucleotide treatments showing promise in animal studies and entering clinical trials to treat so many different genetic diseases. It is especially heartening to see so many efforts in our community to provide solutions for people diagnosed with rare and ultra-rare diseases. Patients with Alexander disease and their families will experience a deep sense of relief knowing there is the hope of slowing the progression of the disease or possibly even experiencing a life free of the devastating symptoms caused by the disease if the current clinical trial of ION373 proves to be safe and effective in humans.
References:
- Alexander Disease. ELA International. (2019, January 17). Retrieved December 10, 2021, from https://elainternational.eu/en/maladie-dalexander
- Messing A. Refining the concept of GFAP toxcity in Alexander disease. J Neurodev Disord. 2019 Dec 16;11(1):27. doi:10.1186/s11689-019-9290-0. PMID: 31838996; PMCID: PMC6913036.
- Messing A. Alexander Disease Research Update – Episode #3 [Internet]. Apple Podcasts, 2021 [cited 2021 Dec 10].
- Ionis Webinar Alexander Disease. https://youtu.be/VkH2YTZfQ24
- Hagemann TL, Powers B, Lin NH, Mohamed AF, Dague KL, Hannah SC, Bachmann G, Mazur C, Rigo F, Olsen AL, Feany MB, Perng MD, Berman RF, Messing A. Antisense therapy in a rat model of Alexander disease reverses GFAP pathology, white matter deficits, and motor impairment. Sci Transl Med. 2021 Nov 17;13(620):eabg4711. doi: 10.1126/scitranslmed.abg4711. Epub 2021 Nov 17. PMID: 34788075.
- Nagata T, Dwyer CA, Yoshida-Tanaka K, Ihara K, Ohyagi M, Kaburagi H, Miyata H, Ebihara S, Yoshioka K, Ishii T, Miyata K, Miyata K, Powers B, Igari T, Yamamoto S, Arimura N, Hirabayashi H, Uchihara T, Hara RI, Wada T, Bennett CF, Seth PP, Rigo F, Yokota T. Cholesterol-functionalized DNA/RNA heteroduplexes cross the blood-brain barrier and knock down genes in the rodent CNS. Nat Biotechnol. 2021 Aug 12. doi: 10.1038/s41587-021-00972-x. Epub ahead of print. PMID: 34385691.








