Looking for something?
The Emerging Era of N-of-1 Drugs for Ultra-Rare Genetic Diseases

Imagine if a medication or therapy could be created to treat just one individual with an ultra-rare disease. There are nearly 7,000 known rare diseases (1) and many are debilitating and ultimately fatal. In the U.S., a disease is considered rare when it affects as many as 200,000 people. In that situation, it is difficult enough to find an accurate diagnosis and treatment. What if you or your child are the only known person with a specific genetic variant causing the disease?
Amazingly, scientific knowledge, technology, and drug development have advanced to the point where the genetic causes of ultra-rare diseases may now be discovered and a drug created for just one patient to be treated, providing hope to these families for the first time in history.
These individualized drugs, called N-of-1 therapies, herald a new era in medicine. Currently, antisense oligonucleotides (ASOs) have been developed furthest and are enhancing the health and quality of life for many people. Perhaps even more importantly, ASOs are providing hope to people with ultra-rare diseases.
The Impact of ASOs in Treating Ultra-Rare Diseases
To understand the potential of ASOs, we first need to understand how DNA information drives the formation of proteins into our bodies.
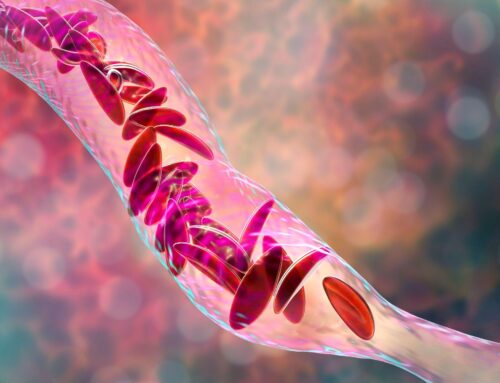
Here is a short and sweet version. Certain sequences of nucleotides in the DNA are transcribed into messenger RNA (mRNA) in the cell’s nucleus, which is essentially the process of passing on information. The mRNA, carrying a specific set of information, leaves the nucleus and enters the cytoplasm where it is translated into proteins. Blocking the translation can alter the production of proteins which opens a new way of making drugs.
Why are these proteins important to target? Well, if mutated proteins are produced (from mutated DNA, in the case of genetic disease), or if too much or not enough of a protein is produced, it is likely to cause disease. Current traditional medications target the harmful proteins but remain complicated to produce.
The problem with this is that it is difficult to target the proteins with current medications or to decrease or increase the amount of proteins made. Additionally, the proteins are already damaging the body, and the damage can be debilitating and irreversible. However, if we can stop the proteins from being made in the first place, or alter the amounts produced, we can stop the process and prevent further damage.
Antisense oligonucleotides (ASOs) can do this. They are short strands of chemically-modified DNA that target and bind precisely with disease-associated RNA to alter the production of proteins (2, 3). By binding to the RNA, they stop the production of the mutated proteins in some cases. In doing so, they prevent the disease-causing protein from being produced, slowing and even halting the progression of the disease. If a disease is caused because not enough of a protein is produced, ASOs can also be used to instruct cells to increase production of that protein. They are chemically modified to increase their binding, and their stability, to allow the effect to take place.
Incredible research efforts have been made to improve the biophysical and biological attributes of the ASOs, making them safe and effective. Numerous ASO drugs that treat an astonishingly wide range of diseases have been approved for use or are in clinical trials. The knowledge gained in developing the drugs for commercial use leads to further avenues in creating ASO drugs for n-of-1 diseases.
Different classes of ASOs are now being used to treat rare and genetic disorders which were previously deemed untreatable (2). In fact, the potential of ASOs is so great that the Oligonucleotide Therapeutics Society (OTS) has put together a Rare Disease N-of-1+ task force to apply ASOs to the treatment of serious, life-threatening diseases affecting less than 100 patients worldwide – to meet unmet needs, while also paving a regulatory path for other platform technologies to follow (3).
ASOs are an excellent avenue for treating genetic disease because the genetic sequences can be customized to a specific mutation (4), they have a good safety profile, and can be developed and manufactured rapidly and relatively inexpensively. Since many patients spend 4-5 years simply trying to find a diagnosis, by the time the cause of their disease is known time is of the essence in creating a suitable treatment.
Milasen was the first personalized ASO approved by the FDA. It was designed to treat Mila Makovec who suffered from a rare, fatal form of Batten disease and its development is an astonishing example of the potential of ASOs in the treatment of those with ultra-rare diseases.
When Mila was 6 years old, neurogeneticist Timothy Yu identified a splicing defect in one of her genes. Knowing that Spinraza is an ASO drug that changes the splicing pattern of a different gene, Yu theorized that a similar ASO could also be used to correct the splicing defect present in Mila’s gene. Using the same chemical backbone and route of administration as Spinraza, within one year Yu and a large team of colleagues identified the appropriate ASO to correct the mis-splicing, tested and confirmed that it was safe in rats, achieved the necessary regulatory approval for an N-of-1 trial, and began treating Mila with the new drug, Milasen (5, 6, 7).
While it did not provide a cure, Milasen undoubtedly slowed the progression of symptoms and improved the severity and frequency of seizures that she experienced (5). “The rapid translation of Milasen from proof-of-concept to clinical use within months is an exceptional and enthusiastic example of the development of an ASO-based precision medicine that can improve a patient’s quality of life by reducing disease severity” (2).
Heartbreakingly, Mila passed on in February of this year, but the path to finding a customized therapy for her set a new precedent in N-of-1 drug discovery and FDA guidelines, altering the trajectory of modern medicine.
Other Encouraging Stories in the Journey of Customized N-of-1 Therapies
Since the creation of Milasen, other patients have benefitted from N-of-1 drugs. Jaci Hermstad was 25 years old in 2019 when she was diagnosed with a rare genetic form of amyotrophic lateral sclerosis (ALS). Her identical twin sister had developed ALS symptoms when they were 11 and died six years later, which spurred Jaci and her family’s drive to find a treatment when she was diagnosed. Their efforts were successful and Jaci received an experimental antisense therapy created by Ionis, called Jacifusen, and was reported to have shown improvement of symptoms before her death (8).
Other children have also received approval for N-of-1 clinical trials using ASOs, including a young girl with ataxia-telangiectasia (A-T). In April of 2020, an update reported that the girl had received six injections of the custom-designed ASO and all safety tests had gone smoothly with no side effects observed.
Regulations Could Be a Roadblock, but the FDA is Working to Make the Process as Smooth as Possible
One challenge that exists for those seeking treatment for ultra-rare diseases lies in working with regulatory agencies and gaining approval to try novel drugs. In the United States, we have the U.S. Food and Drug Administration (FDA) whose mission is to protect public health, in part by ensuring that drugs are both safe and effective before they are approved for use in humans. Most other countries have a similar agency in place. While these agencies do play a vital role in protecting citizens, it also creates an extra level of bureaucratic red tape for patients and families desperate to find an immediate solution. Fortunately, the FDA is working to allow patients to more swiftly and easily receive these types of treatments.
In the case of Milasen, it had the same chemical backbone and was administered in the same way as Spinraza, which had already gained FDA approval. This expedited the process of toxicity testing, obtaining authorization from the Food and Drug Administration (FDA), and gaining institutional review board approval to conduct an N-of-1 clinical trial as there was already a precedent in the approval of Spinraza.
Since the creation of Milasen, other individualized ASO drugs have been created and requested regulatory approval for an N-of-1 clinical trial. Recognizing the growing impact that N-of-1 drugs will have in the future, the FDA released a statement providing clarity on developing new, individualized drug products in which they state that “the FDA understands that we’ll need to work together with the developers of these drug products to bring them safely to patients, and we are willing to engage as needed to address the challenges” (FDA). They have been proactive in creating guidelines and, in January of 2021, released guidance for Submissions of Individualized Antisense Oligonucleotide Drug Products.
The Financial Burden of Individualized Drugs
As you can imagine, creating Milasen was an extremely expensive endeavor. Drugs for rare diseases often cost hundreds of thousands or even millions of dollars. Mila’s mother, Julia Vitarello, raised $3 million to fund research into Batten disease and fund the development, manufacturing, and toxicity testing of Milasen (6). She also started Mila’s Miracle Foundation whose focus has now turned to finding and funding paths to a cure for devastating neurological conditions and make these personalized medicines accessible. However, fundraising on this scale is not possible for most families of patients with rare diseases.
This truth is displayed in the title of a recent article in MedPage Today “Desperate Families Pursue ‘N-of-1’ Trials for Ultra-Rare Diseases – Technology dangles hope of cure — for those able to pay.” The article tells the stories of Jaci Hermstad and Mila Makovec, and the effort that went into fundraising and gaining FDA approval. Although the FDA has worked to streamline the process for N-of-1 clinical trials, while maintaining commitment to quality and safety, the high cost associated with customized drugs is not a problem that is easily solved.
A sad truth in the history of modern medicine has been that research money went to diseases that affected a large number of the population. Until recently, knowledge of science and medicine combined with limited resources contributed to this fact. However, we are entering a new era in which N-of-1 therapeutics are a reality and financial solutions need to be created so that money does not prevent a candidate from receiving an individualized drug that could prolong and improve their life.
Filling the Gap for Families of Patients with Ultra-Rare Diseases
Many non-profit organizations exist to provide resources for people with rare diseases. A new type of organization was created a year ago in the n-Lorem Foundation. n-Lorem is the first and only nonprofit organization whose mission is to create experimental antisense oligonucleotide (ASO) treatments for patients who have diseases caused by extremely rare mutations and provide these treatments for free, for life.
It was created by Dr. Stanley Crooke, who is also the founder of Ionis Pharmaceuticals, a biotechnology company that specializes in discovering and developing RNA-targeted therapeutics. Ionis has 3 commercially approved medicines, all of which are antisense therapeutic oligonucleotides. n-Lorem leverages the powerful ASO technology developed by Ionis Pharmaceuticals to provide high-quality, personalized ASO therapies.
n-Lorem has made extraordinary progress in offering hope and rapid personalized treatment to patients affected by ultra-rare mutations during its first year of operation. The foundation received 50 applications and, incredibly, nearly 20 of the applicants were good candidates for individualized ASO treatment and are in the process of receiving treatment.
The Foundation not only creates and provides customized ASO treatments but is also developing a broad network of collaborations to assure that n-of-1 patients receive the highest quality experimental ASO treatments as rapidly as possible, at the lowest cost per patient, so they can meet the needs of as many patients as possible.
They have created quality, detailed processes and evaluations. Cutting corners when it comes to quality processes will not only be detrimental to everyone involved but will have the most damaging effect on future patients who need this type of treatment. The foundation is also working with the FDA to develop definitive guidance that facilitates meeting the needs of these patients with the highest possible quality.
Why would the founder of a pharmaceutical company begin a non-profit like n-Lorem?
As Stan Crooke explained, “n-Lorem is a great opportunity to do something good for families in need and our industry. n-Lorem shows the true heart of the pharmaceutical/biotechnology industry.” Nothing displays this true heart more than the passion and empathy in his voice when he talks about parents of these children just wanting hope and more time with their children or when he said that his dream for n-Lorem is to “help a single patient and a single family, one family at a time. That will change the world, too, and change the future of the patient and these families.”
To learn more about the progress n-Lorem has made in its first year, and the care and effort that goes into providing customized ASOs for people with ultra-rare diseases, watch this webinar.
Providing Hope
Oligonucleotide therapies have a far greater potential for the treatment of rare diseases than current drugs and offer priceless hope to patients and their families. Rare diseases affect between 263 – 446 million people around the world at any given time. 71.9% of the known rare diseases are genetic and 69.9% are exclusively pediatric onset (1). Many of these diseases take a significant amount of time to diagnose and do not have approved treatments. This means somewhere between 184 million to 312 million children are suffering from a rare disease, with families who are searching desperately for hope for their child’s future.
Mila Makovec’s story displays the astonishing possibilities when a parent’s determination aligns with emerging science and brings hope to families with children diagnosed with ultra-rare disorders. As knowledge and technology advance, perhaps someday every single person with an ultra-rare disease will gain access to effective and life-saving treatments.
References:
- Nguengang Wakap, S., Lambert, D.M., Olry, A. et al.Estimating cumulative point prevalence of rare diseases: analysis of the Orphanet database. Eur J Hum Genet28, 165–173 (2020). https://doi.org/10.1038/s41431-019-0508-0
- Dhuri, K., Bechtold, C., Quijano, E., Pham, H., Gupta, A., Vikram, A., & Bahal, R. (2020). Antisense Oligonucleotides: An Emerging Area in Drug Discovery and Development. Journal of clinical medicine, 9(6), 2004. https://doi.org/10.3390/jcm9062004
- OTS – Aartsma-Rus, Annemieke, et al. “OTS Rare Disease N-of-1+ Workshop Briefing Document.” Oligotherapeutics.org, Oligonucleotide Therapeutics Society, www.oligotherapeutics.org/wp-content/uploads/2020/11/OTS-N-of-1-Briefing-Doc_April-23_KG-AR_FN051220.pdf.
- Hagedorn PH, Yakimov V, Ottosen S, et al. Hepatotoxic potential of therapeutic oligonucleotides can be predicted from their sequence and modification pattern. Nucleic Acid Ther 2013;23:302-310.
- Kim, J., Hu, C., Moufawad El Achkar, C., Black, L. E., Douville, J., Larson, A., Pendergast, M. K., Goldkind, S. F., Lee, E. A., Kuniholm, A., Soucy, A., Vaze, J., Belur, N. R., Fredriksen, K., Stojkovska, I., Tsytsykova, A., Armant, M., DiDonato, R. L., Choi, J., Cornelissen, L., … Yu, T. W. (2019). Patient-Customized Oligonucleotide Therapy for a Rare Genetic Disease. The New England journal of medicine, 381(17), 1644–1652. https://doi.org/10.1056/NEJMoa1813279
- Mullard A. N-of-1 drugs push biopharma frontiers. Nat Rev Drug Discov. 2020 Mar;19(3):151-153. doi:10.1038/d41573-020-00027-x. PMID: 32127676.
- Cross, Ryan. “Milasen: The Drug That Went from Idea to Injection in 10 Months.” C&EN, Chemical & Engineering News, 16 Oct. 2019, cen.acs.org/business/Milasen-drug-idea-injection-10/97/i42.
- Dolgin, Elie. “News Feature: Gene therapy successes point to better therapies.” Proceedings of the National Academy of Sciences of the United States of Americavol. 116,48 (2019): 23866-23870. doi:10.1073/pnas.1918306116
- Cavazzoni, Patrizia. “FDA Takes Steps to Provide Clarity on Developing New Drug Products in the Age of Individualized Medicine.” U.S. Food and Drug Administration, FDA, www.fda.gov/news-events/press-announcements/fda-takes-steps-provide-clarity-developing-new-drug-products-age-individualized-medicine.