Looking for something?
Oligonucleotides Provide Hope for the Treatment of Duchenne Muscular Dystrophy

Imagine if your muscles began weakening for no apparent reason. Then, after an ongoing search for a diagnosis, you learn that you have a disease in which your muscles would progressively waste away and become weaker until you would no longer be able to walk. Ultimately, the disease would lead to death. This is exactly what people diagnosed with various forms of muscular dystrophy experience.
Although most forms appear during childhood, some are congenital, while others affect adults. There are currently no cures, and various treatments only help manage symptoms and improve quality of life. However, since muscular dystrophy is caused by defects in certain genes, oligonucleotide therapeutics may be the key to developing effective treatments. In fact, we have recently seen the development of multiple oligonucleotide drugs, and even a few approvals by the FDA, to treat this devastating group of diseases.
There are more than 30 types of muscular dystrophy, and Duchenne Muscular Dystrophy (DMD) is the most common. DMD usually affects males, and symptoms appear between the ages of 1 and 6. Sadly, one out of every 3,500 – 4,000 males will receive a diagnosis of DMD.
Researchers first discovered that DMD has a genetic cause in 1986 (1). It occurs when there are mutations in the gene that codes for a protein called dystrophin. Depending on the mutation, cells either fail to make any functional dystrophin or only make a very small amount. Since DMD is one of the largest genes in humans, containing 79 exons, it is highly susceptible to mutations (2, 3).
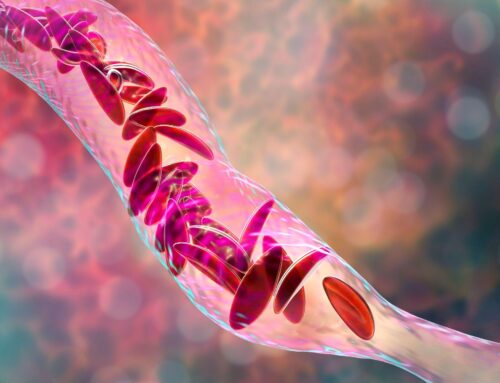
Dystrophin is part of a protein complex that provides structural support to muscle fibers, strengthening them and providing protection to the muscle fibers. The absence of dystrophin means that every single time a muscle is contracted it can be damaged, leading to progressive muscle deterioration. It is eventually fatal because all types of muscle tissue are affected, including that of the diaphragm and heart.
In another form of muscular dystrophy, Becker muscular dystrophy (BMD), different mutations in the same gene allows some partially functional dystrophin to be made, but not enough to avoid symptoms. This does allow symptoms to be noticed much later, usually as an adult, and progress much more slowly than in DMD. Other forms of muscular dystrophy impact specific muscle groups and vary in severity, but all result in muscle deterioration, and most do significantly decrease life expectancy.
Antisense oligonucleotides have received approval to treat Duchenne Muscular Dystrophy.
Approximately 60-70% of cases of DMD are due to deletions of one or more exons, with the rest being due to duplications or other mutations (2, 3). The deletions can cause a disruption of the protein’s reading frame, resulting in a premature stop codon. Antisense oligonucleotides are an excellent candidate for treating this type of mutation because they bind to the part of the RNA that has missing or mutated exons, blocking the translation of that sequence. Since this causes the cells to skip over the mutated exon, it is considered an exon skipping therapy. Bypassing the mutated exon repairs the reading frame, which allows for the creation of shorter, yet functional dystrophin (3).
Several antisense oligonucleotides are in development to treat DMD through exon-skipping, and four have been approved. Each drug skips one specific exon, so patients who have a confirmed mutation amenable to skipping of those exons may benefit from treatment.
Sarepta Therapeutics has gained FDA approval for three of the four approved ASO drugs to treat DMD. Exondys 51 (eteplirsen) binds to exon 51 and approximately 14% of patients with DMD have a mutation of this exon (4). It was approved in 2016, becoming the first exon skipping drug to receive FDA approval.
Vyondys 53 (golodirsen) was the second to receive FDA approval, which it gained in December of 2019. It binds to exon 53, and up to 10% of all DMD mutations are amenable to exon 53 skipping (4).
The third ASO drug developed by Sarepta to treat DMD Amondys 45 (casimersen) binds to exon 45. It just recently received FDA approval on February 25, 2021. Approximately 8% of patients with DMD have a mutation of exon 45 (4).
NS Pharma developed a fourth ASO drug for the treatment of Duchenne Muscular Dystrophy, which gained FDA approval in August of 2020. NS Pharma’s Viltepso (viltolarsen) binds to exon 53 as does Golodirsen. Although Viltepso gained approval eight months later than Golodirsen, it may have an advantage since it is 4 nucleotides shorter than Golodirsen, which may lead to a greater increase of dystrophin.
All four of these result in an increase of dystrophin in skeletal muscle, however, it is unclear yet whether this results in clinical benefit, including improved motor function or slowing the progression of the disease. The drugs received accelerated approval, which is conditional based on outcomes of further clinical trials. Multiple trials are still ongoing for these drugs, to determine if higher doses lead to more therapeutic effects, to evaluate if restoring dystrophin in patients in less advanced stages of the disease will have a greater impact, and to determine safety in more advanced cases of the disease.
Just this month, Sarepta announced the results of a Phase 2 trial of SRP-5051, a second-generation exon-skipping drug intended to treat the same patients as Exondys 51. Data from four patients showed that monthly administration (rather than weekly infusions required by Exondys 51) provided much greater gains in dystrophin levels than current treatments. Unfortunately, reduced magnesium levels were a severe side effect observed in two of the four patients, but the effects were reversed by supplementation of oral magnesium.
Each of the drugs listed above skips one exon. Since mutations can span more than one exon, it may be possible to create a cocktail of ASOs that could potentially treat a far greater number of patients with DMD (5).
Other promising oligonucleotide therapies to treat muscular dystrophy.
One concern in treating DMD is in delivering ASOs to cardiac tissue. If skeletal tissue is strengthened it can actually increase the rate of deterioration of the heart unless the cardiac tissue is also restored. There are many interesting avenues being explored to deliver ASOs to the heart, including polymers, nanoparticles, conjugation to cell-penetrating peptides, and even using a combination of microbubbles and ultrasound (2).
Pfizer has developed a gene therapy using an adeno-associated virus (AAV9) capsid to deliver a shortened dystrophin gene to muscle cells. A benefit to this gene therapy is that all mutations can potentially be treated. On January 7, 2021, Pfizer announced that the first participant of a phase 3 trial was dosed. The primary goal of this study is the change from baseline in the North Star Ambulatory Assessment (NSAA) at one year. The NSAA measures gross motor function in boys with DMD and earlier studies found either improvement or stable NSAA scores, which is far outside the norm. This study is evaluating the therapy in boys from 4 to 7 years old who can still walk a short distance on their own, but Pfizer is also planning a second Phase 3 study to evaluate it in men with DMD who cannot walk without assistance.
In contrast to the forms of muscular dystrophy that will respond well to exon skipping, others are caused by improper protein production and may respond well to RNAi therapies. Limb-girdle muscular dystrophy (LGMD) is a group of similar muscular dystrophies with different genetic causes that are grouped into two types. One type is caused by the production of abnormal proteins. Therefore, RNAi may also be an effective therapy for this type and labs are currently researching this.
Oculopharyngeal muscular dystrophy (OPMD) is due to a defect in the PABPN1 gene and most often causes muscle weakness around the upper eyelid and pharynx. Benitec Biopharma is developing an experimental treatment that combines RNAi to bind to the mutated PABPN1 mRNA, preventing it from producing the mutated protein, while also introducing a healthy copy of the PABPN1 gene. Benitec hopes to initiate the first in-human study in 2022.
Continued development of oligonucleotide therapies provides hope for effective treatments.
Muscular dystrophies are devastating to patients and their families and are particularly challenging to treat since a wide array of mutations cause them. The recent approval of a fourth ASO to treat Duchenne muscular dystrophy provided another avenue of hope, and many other therapies are being investigated in the desire to provide relief to these families. Perhaps one of the avenues of investigation will even produce a cure in the near future.
References:
- 1. Hoffman EP, Brown RH Jr, Kunkel LM. Dystrophin: the protein product of the Duchenne muscular dystrophy locus. Cell. 1987 Dec 24;51(6):919-28. doi: 10.1016/0092-8674(87)90579-4. PMID: 3319190.
- 2. Nguyen Q, Yokota T. Antisense oligonucleotides for the treatment of cardiomyopathy in Duchenne muscular dystrophy. Am J Transl Res. 2019 Mar 15;11(3):1202-1218. PMID: 30972156; PMCID: PMC6456507.
- 3. Gao QQ, McNally EM. The Dystrophin Complex: Structure, Function, and Implications for Therapy. Compr Physiol. 2015 Jul 1;5(3):1223-39. doi: 10.1002/cphy.c140048. PMID: 26140716; PMCID: PMC4767260.
- 4. Schneider AE, Aartsma-Rus A. Developments in reading frame restoring therapy approaches for Duchenne muscular dystrophy. Expert Opin Biol Ther. 2021 Mar;21(3):343-359. doi: 10.1080/14712598.2021.1832462. Epub 2020 Oct 19. PMID: 33074029.
- 5. Himič, V., Davies, K.E. Evaluating the potential of novel genetic approaches for the treatment of Duchenne muscular dystrophy. Eur J Hum Genet (2021). https://doi.org/10.1038/s41431-021-00811-2